Bio-convergence
A quantum leap In the drug development world
Microfluidic chips that simulate human tissue enable us to conduct medical experiments in ways that could not have been even imagined only a few years ago. Two leading Israeli researchers report from the turbulent Israeli front line of the global 'organ-on-a-chip' sector
'Laboratory-on-a-chip,' that is based on microfluidics, enables us to simultaneously conduct multiple and complex sets of experiments that generate a high data output such as a survey of biochemical, physical and cell data, with a tremendous saving in the number of samples required and the duration of the experiment.
 Bar Ilan University. Photo: Yariv Katz
Bar Ilan University. Photo: Yariv Katz
Prof. Doron Gerber is a researcher in the Nanotechnology Center and Faculty of Life Sciences at Bar Ilan University. "My background is in biology," he says. "After a doctorate that examined membranal proteins, I decided to do something of a more technological nature. I completed a post doctorate with Prof. Stephen Quake at Stanford – a researcher who introduced me to the whole field of controlled microfluidics. Prof. Quake invented a new type of microfluidics that enables us to conduct extremely complex experiments and to develop applications in the fields of biology, chemistry, and physics by using flexible switches that enable complete control of whatever happens inside the chip. In other words, the technology allows smart management of small nano-liter quantities of fluids.
"How does it all work? Let's say that we want to conduct 1,000 simultaneous experiments. First, we need a sample of the substance we are studying such as, a drop of blood. In regular experiments, we only have a limited number of available samples, either because they are taken from a single person or because they are very expensive.
"Microfluidics allows us to perform complex procedures with tiny amounts of samples. Let's imagine that I had an endless quantity of blood to examine: I would take 1,000 test tubes and attempt to perform one experiment using different substances on a blood sample in each one according to the parameter I wanted to test.
"Here, we miniaturize the experiment set so that we have 64 micro-cavities instead of test tubes. Each of these cavities contains only one-thousandth of a drop of the patient's blood. Each cavity is one quarter of a square millimeter and is 20 microns high, so its volume is only a few nano-liters (1 nano-liter is one millionth of a liter). The passages between the micro-cavities are canals, each up to a hairbreadth wide, through which the substances required for the different experiments move. Multiply this set by 64 levels and you can conduct thousands of experiments at the same time.
 Blood tests. Photo: Shutterstock
Blood tests. Photo: Shutterstock "To make it work, we need each experiment to remain separate from the others, so we created a 'door' that in addition to separation also allows us to insert and extract things. This door is an elastic switch that opens and closes according to instructions given from a computer software.
"In other words, our microfluidic chips are set of extremely small cavities and a system of fully controlled switches ('doors') capable of timed insertion and extraction of substances from the cavities. An experiment set like this can be used in a wide range of scientific experiments such as searching for substances in the blood like antibodies, pieces of DNA or RNA from a viral source, indicators of cancer etc. A small volume of a patient's blood can be used as a sample, inserted into the chip so that each of the chip's many cavities contains a small drop of blood and can 'host' a test to locate the substance under examination, enable its quantification, or a qualitative analysis that indicates its presence in the blood.
"In other experiments, such as those that check the connection between proteins of different viruses and human proteins, we can start from the level of the genetic material of a person or a virus, translate it into proteins that are given fluorescent markers (fluorophores) in the chip's cavities, and evaluate the degree and strength of the connection created between these proteins. Information such as this is extremely valuable in studying viruses' operating mechanisms and the way they influence human cells. Finding a strong connection between a viral protein and a human protein hints to the involvement of these proteins in the way the virus infects or spreads and can therefore constitute a target site for the development of a treatment for that virus.
"In addition to working with different molecules, the microfluidic platform also enables us to work with whole cells.
"In the field of cancer research, there is a good correlation between the results of the laboratory experiment and clinical results. Nevertheless, the main problem is that a sample taken from a cancer patient contains many cancer cells and there is no way to cultivate them in such a way as to be able to conduct dozens of experiments and analyze their influence on a range of possible treatments. In an attempt to overcome this obstacle, scientists are trying to grow the tumor cells in the lab and increase their number and only then expose them to different treatments, but this is a race against time.
"We have developed a microfluidic chip for culturing the cells. Each of the chip's cavities can accommodate a tiny quantity of cancer cells taken from a specific patient and allows us to expose each group of cells to a different pharmaceutical treatment and check their reaction to it. This method enables us to know which treatment the cancer cells are resistant or sensitive to and how they respond, all within just a couple of days.
"Although there are currently many drugs for treating cancer, it's not clear how each patient will respond to each of them. A specific drug may cause harsh side effects and be ineffective in treating the disease so the window of opportunity for treating these patients is extremely limited. The results of an experiment using our chip can help direct the patient's physician to choose the most efficient treatment for him, thereby saving precious time and unnecessary suffering.
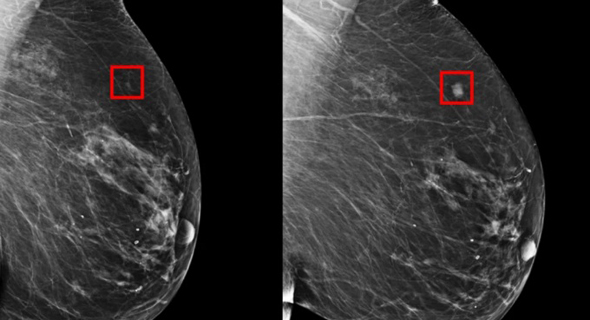 A canserous tumor. Photo: MIT
A canserous tumor. Photo: MIT "A year ago, we published an initial paper in which we proved the theory and presented the system's capabilities. We have now begun checking patient samples. The paper gained considerable interest, and many have expressed a wish to examine samples using our system.
"We recently began collaborating with Dr. Amir Onn, Head of the Institute of Pulmonary Oncology at the Sheba Medical Center and Dr. Limor Broday from Tel Aviv University. The time limit with lung cancer is especially short. From the moment the patient stops responding to treatment, a doctor needs to receive the relevant knowledge and make a very quick informed decision regarding alternative treatment. In our joint study, we attempt to assess whether our method can facilitate a swift and accurate decision, thereby enhancing the results of the treatment administered to the patient.
"There is a tremendous need in this field, and we are attempting to get financing from scientific grants that will enable us to survey about 300 patients over the next two years. This will, in turn, allow us to characterize the system in relation to a set of lung cancer medications while simultaneously upgrading the system that checks the vitality and mortality data following exposure to the medication. In the future, we hope to add a further capability to the system that will facilitate the measurement of metabolic indices which report on processes within the cells such as glucose and energy levels, and that provide more in-depth information.
"The device's complexity means that the need for large-scale investment is a fundamental issue in the chips' production processes. Our dream is to enable biologists to take an idea and bring it to engineering implementation: lab production of a chip. This for me is the essence of Bio-convergence – a biologist using sophisticated engineering to create innovative solutions.
"We built a factory at Bar Ilan University for producing microfluidic chips, not only for my laboratory but also for additional labs at Bar Ilan and other institutions as well as for Israeli industry, but we belong to academia and it's only a small factory with limited human and financial resources. As of now, our largest challenge is to enable industry to utilize the potential of the infrastructure we have constructed,” he said.
The Future of Microfluidics
Prof. Gerber predicts a rosy future for the tiny chips: "It's happening all around the world – microfluidics is entering the world of diagnostics and the field of developing tools for scanning medications and substance synthesis e.g., therapeutic antibodies or antibodies for genetic engineering of viruses etc.
"The industry needs microfluidic chips to produce therapeutic antibodies and to market them as drugs and increasingly more microfluidic tools are appearing in manufacturing or development processes. As of now, this kind of research only exists on a small scale in Israel, primarily in academia, with large-scale microfluidic centers needed to integrate the technology into the industry. If, for instance, we assume that a startup company receiving a limited initial sum of money wants to use a microfluidic tool, its chances of success are slight. Among the reasons for this is the lack of appropriate infrastructures – production of a simple microfluidic chip requires a manufacturing plant with clean rooms, equipment for creating molds by lithographic processes, equipment for coating molds, and equipment for producing the chips.
"Today, when it is obvious to everyone that there is a need to connect biology and high-tech, it is also clear that most of the major tools for doing so actually exist in academia far more than in industry. On the other hand, academia lacks the large-scale infrastructures required to transform technology into an off-the-shelf product like production of a chip prototype. Since entering academia, I have established, and am still establishing, a microfluidic chip center capable of producing different kinds of chips and providing support to new researchers seeking to make use of microfluidic technology, all subject to the limitations of the existing support in academia.
"There is no doubt that large-scale investment and significant financial incentives directed at the development of basic infrastructures are required for the field of microfluidics to transcend the walls of academia and penetrate industrial realms. In contrast to biology for example, where you can buy a robot to perform large quantity tasks, microfluidics is characterized by a scarcity of companies that develop these tools for others. Investment in this infrastructure will enable companies to make use of off-the-shelf products and to integrate these innovative technologies into their applications. Young industry must also be connected to academic capabilities.
"Many companies who come to our nanotechnology center for example, use our equipment and at the same time, receive good counseling. But this happens at an academic pace. We must invest a little more in this infrastructure so that it serves industry better, for example, in the establishment of a consortium which we aspire to be a member of."
Dr. Itai Kela, Scientific Director of the Bio-Convergence Program:
"The integration of microfluidics used for discovering new medicines and 'lab-on-a-chip' systems creates an amazing technology that enables to dramatically reduce the use of lab animals when developing drugs and constitutes an engineering technological platform for the scanning and more rapid and efficient detection of new medicines and treatments."
The Sensors that Discover Why Medications Fail
When discussing Bio-convergence and the combination of industry and academia, it is important to learn about the work of Prof. Yaakov "Koby" Nahmias. Prof. Nahmias, Founding Director of the Bioengineering Center at the Hebrew University in Jerusalem, is a serial entrepreneur and Chief Scientist of the Tissue Dynamics corporation which he founded a year ago.
 Prof. Yaakov Nahmias. Photo: Orel Cohen
Prof. Yaakov Nahmias. Photo: Orel Cohen "Bio-convergence – the structured combination of engineering biology and medicine – is a very important part of projects' technological maturity and enables amazing breakthroughs," he says. "In practice, one of the main reasons behind the establishment of the Bioengineering Center at the Hebrew University was the desire to provide an academic response to the growing need for engineers who understand biology and vice versa."
As an example of the importance of Bio-convergence, Prof. Nahmias relates to the coronavirus: "When the 'Hepatitis C' virus was discovered in the year 2000, it took 3-4 years to sequence it and then an entire year to grow it. The first medication arrived only several years later. In other words, it took about a decade to develop molecules capable of contending with 'Hepatitis C'.
"In contrast, the new coronavirus was only discovered in November and was more or less sequenced already in December. Its first tissue cultures were ready in January-February with the first molecules being introduced to clinical research around March. What took years with 'Hepatitis C' is being done in just weeks and a few short months with Covid-19. This is much more than an exponential increase – it's a quantum leap.
"Today's world moves extremely fast and investors need to take into account that the pharma industry is going to reverse itself. The 1970s and 1980s were characterized by a lot of mediocre pharma companies, most of which were swallowed up by a small number of pharma giants that are the only ones with the massive resources necessary to bring a new drug to the market. The next technological revolution will enable an entire community of small pharma companies to compete with the giants.
"I am a member of the Innovation Authority's Bio-convergence Committee that will lead a dramatic breakthrough in Israel's technological capabilities. The Authority helps the academic world penetrate industry, receive necessary resources, and transform theoretical solutions into practical applications. If until 15 years ago the world of academia was extremely theoretical and did not view the connection with industry as something positive, I believe that this view has changed over the last decade. Today, both the universities and their academic staff are very interested in industry and are working closely with the Authority. The attitude has changed even more in recent years during which young faculty members are themselves beginning to lead startup companies to the market and I hope that this trend will continue,” he said.
Tissue Dynamics operates in the 'organ-on-a-chip' field and seeks to change the world of pharma development.
"Drug development is a long and high-risk process," Prof. Nahmias explains. "2.6 billion dollars and 10-12 years are required to bring a new drug to the market. For each molecule that reaches the medical market, there are 90 others that fail despite the huge resources invested in them. Every molecule that fails at the animal testing stage or in clinical trials costs hundreds of millions of dollars. Drugs sometimes fail even after FDA approval, release to the market, or administration to patients.
 Laboratory trials. Photo: Pixabay
Laboratory trials. Photo: Pixabay "This is the reason that although there are hundreds of companies developing pharmaceuticals in Israel, none of them has the resources to reach the market. These companies will eventually be sold to a pharma giant which will then conduct the final clinical trials. This reality limits Israel's ability to compete with other countries.
"One of the main reasons that drugs fail is that we develop them on animals. We have drugs that work well in mice but not in humans. Another problem is that we don't understand precisely why a drug fails clinical trials. It's a kind of black box that means we can't just change the molecule and move forward – we have to start again from the beginning. That's why pharmaceutical development is such a Sisyphean, costly and long process.
"The 'organ-on-a-chip' story began more than a decade ago when an entrepreneur approached my lab at Harvard to ask for help with developing the technology. The idea is to take human cells – with human genetics and metabolism – and place them on a microfluidic chip that simulates human physiology in order to grow tissues of different organs. The microfluidic chip is made of plastic and is about the size of a 5-shekel coin. Instead of conducting an experiment on a rat or a mouse, we use a microfluidic chip containing tiny tissues of human organs.
"I am very interested in this field and I developed the first 'organ-on-a-chip' technology that was commercialized for an American company called HuREL. Although the technology met the need for human trials, it didn't solve the second problem – attaining a clear understanding of why a drug doesn't work.
"When I returned to Israel to set up the bioengineering center, I focused on the attempt to solve both problems simultaneously. For five years, we developed a technology that enables us to take human cells, use them to create human liver, heart, brain and kidney tissues, and to insert into them sensors that allow us to measure the tissues' activity in real time. This in turn gives us the ability to discover what happens to human tissue when we give it a drug or during a disease.
"The sensors operate exactly as they do in a motor vehicle: if the vehicle shuts down, the oil warning light flashes and we understand the problem. When I administer a drug to healthy tissue that suddenly stops working, I know precisely where that molecule has hit. If I insert a molecule into a heart in which I identify a disease and it restores the regular heartbeat, the sensors show me why it works.
"This technology enables us to completely alter the world of pharmaceuticals. It can reduce development costs up to 80% which means that it will be possible to develop a drug from scratch and bring it to the market for the cost of a few hundred million dollars. This has tremendous significance for the Israeli economy. Hundreds of Israeli pharma companies may not be sold but rather, reach the market by themselves."
The Road to Decentralizing Drug Development
Tissue Dynamics was founded two years ago. As Prof. Nahmias explains: "we started out as a small company, without any external funding. We gave giant companies like L'Oréal, Merck, and Teva access to our technology so that they would understand its potential. Several months ago, just before the Corona crisis, we embarked on a funding round for initial investments.
"We are currently at the stage of slowly moving out of the university. We have independently developed new molecules for treating arthritis and cancer and are now taking our platform in the direction of a new model of drug development. This is Tissue Dynamics' second and more mature corporate stage.
"Our overall vision is of a decentralized drug development structure: a cloud-based smart learning program that has access to several Tissue Dynamics systems distributed between leading labs around the world. The primary platform is situated at our company where we are developing new biological and molecular models but also forging contacts with leading labs worldwide and assimilating our technologies there. These contacts allow us to create biological and chemical data and information that are not just ours, and to include information from other groups worldwide. Our first collaboration in the US is with ATCC (American Type Culture Collection), the world's largest cell and tissue database. ATCC has about 4,500 human tissues from healthy and sick people and access to such information allows us a much deeper understanding of the different mechanisms.
"Six months ago, we developed a new model of the human kidney that enables us to observe a drug's activity and toxicity in the kidney. One of the drugs we examined is called cyclosporine and is given to patients who received organ transplants or who suffer from arthritis. Cyclosporine generates global sales revenues of approximately 4 billion dollars a year despite the known fact that it causes kidney damage.
"When we inserted the drug into a kidney, the sensors were activated and provided us with an energy map of how the drug behaves in a human kidney. Strangely, it turns out that it activates the same mechanism as that in a fatty liver. Nobody knew about this mechanism previously and it was impossible to see without our sensors. This breakthrough meant that we could perform a quick reformulation of the drug and reduce its toxicity. We believe that this constitutes a revolutionary breakthrough in drug development."
The article was written in collaboration with the Israel Innovation Authority, responsible for the country’s innovation policy. Its role is to nurture and develop Israeli innovation resources, while creating and strengthening the infrastructure and framework needed to support the entire knowledge industry.



